Brain Surgery: a Promising Treatment for Drug Addiction
Photo Credit: Greg Ellis/WVU Photo VIA WVU Today
With multiple successful clinical trials, a promising new treatment for substance use disorder takes the form of two thin wires inserted into two different parts of the brain that administer electrical stimulation deep inside.
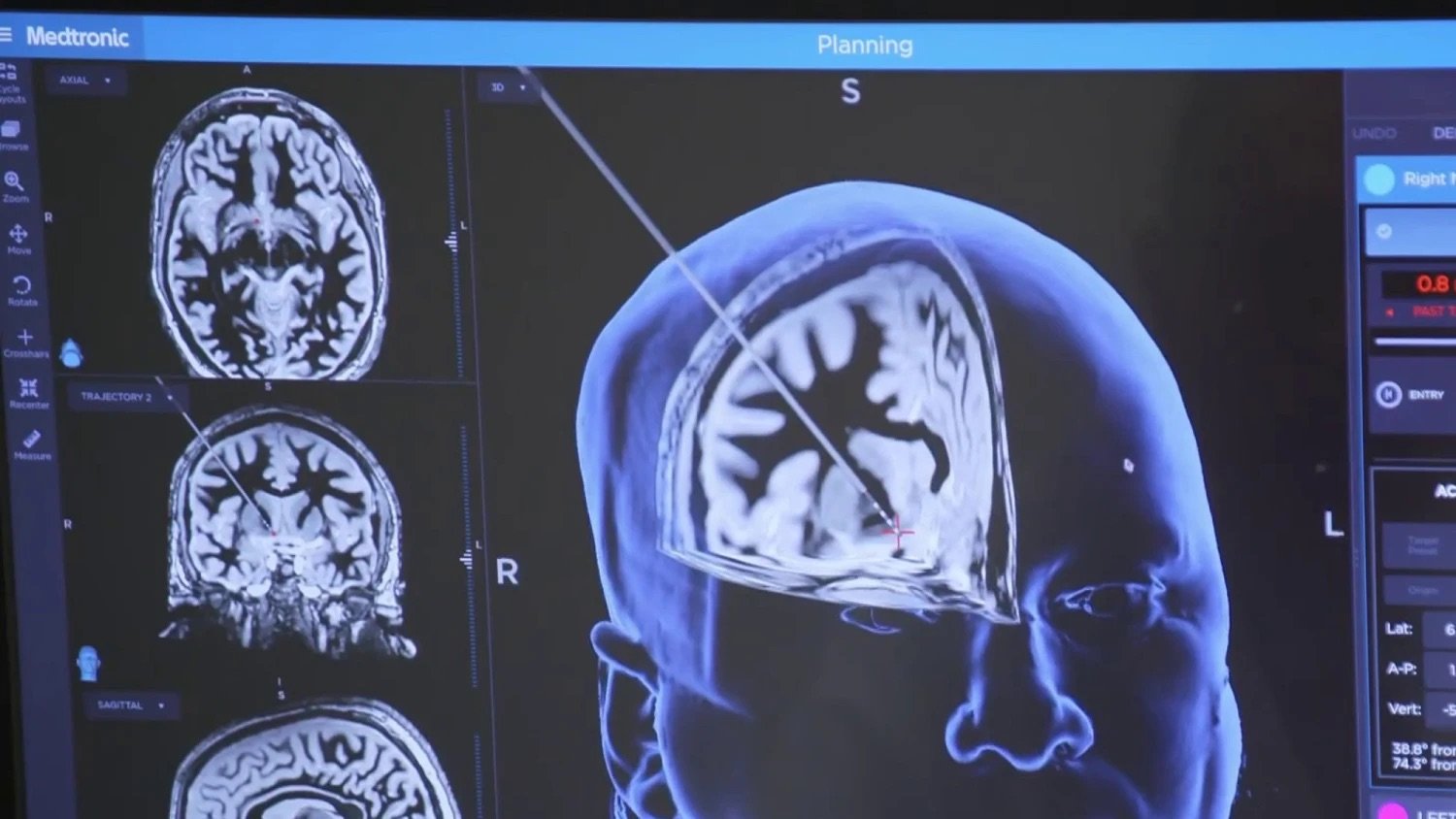
On the morning of Nov. 1, 2019, Dr. Ali Rezai, neurosurgeon and neuroscientist at West Virginia University’s Rockefeller Neuroscience Institute, introduced a novel form of drug abuse treatment in clinical trials known as Deep-Brain Stimulation (DBS). The procedure began with the surgeon drilling two nickel-sized holes in the patient’s cranium and inserting thin probes with four electrodes each into two regions of the brain: the nucleus accumbens and the prefrontal cortex.
According to Dr. Rezai, drug addiction is caused by permanent neurological changes to the activation of part of the brain known as the mesolimbic pathway, which includes the nucleus accumbens and is responsible for the transfer of dopamine to parts of the brain.
“The nucleus [accumbens] becomes overactive, to seek the dopamine [as a result of opioid addiction],” he explained in an interview with CNN, also stating that the prefrontal cortex, a region of the brain responsible for decision making, is “less active.”
Although the addiction-prevention mechanism of DBS is still under investigation, researchers have theories for its effectiveness. Research from Dr. Urbano from the University of Buenos Aires, and Dr. Hashimoto from Aizawa hospital’s Department of Neurology, suggests that DBS slows the activity of the nucleus accumbens while promoting activity in areas connected to the region, reducing the patient’s desire for high levels of dopamine.
Another possible mechanism lies in the reversal of addiction-generated neuroplasticity, the brain’s aptitude in creating new neural connections and rearranging previous ones. According to neurologist Meaghan Creed from Washington University, with the presence of a dopamine receptor dampener, DBS targeting the nucleus accumbens was effective at reducing the enticement of cocaine for long periods of time, meaning that the treatment had reversed previous neural links caused by addiction.
With the implantation of the DBS device inside the brain, Dr. Rezai’s team is able to direct the device to administer electrical stimulation at precise timings, frequencies, and voltages. Additionally, the researchers provided 24/7 support regarding the DBS device to patients, and they adjusted the location and power of the stimulation if patients described feeling discomfort.
In March 2021, after over a year of treatment, the implant in the first recipient of DBS treatment was replaced in favour of a similar one with an additional electrical sensor to detect neuroelectrical activity and signalling. Gerod Buckhalter, the 35-year-old recipient who was previously an opioid addict for 17 years, has been clear of addiction since his first treatment; whereas prior to his treatment, he had not been able to maintain sobriety for over three months.
A month later, Buckhalter was put into an MRI machine to further examine his brain activity, and without his knowledge, the research team turned off the DBS stimulator. Over the next three days, the researchers showed him drug-consumption-related images and noticed a relapse of symptoms that plagued him before treatment, such as anxiety and drug craving.
After switching the DBS back on, neuropsychologist James Mahoney noted that all of these symptoms improved drastically. “You could tell [how much it helped],” he said, noting that Buckhalter’s body had “shifted.”
Photo Credit: West Virginia University VIA NBC News
His life “just felt better,” Buckhalter explained in an interview with CBS. “I just felt like I did prior to ever using drugs, but a little bit better,” he said, claiming that he “knew [he] was gonna have a legitimate shot at doing well.”
As of January 2024, out of four patients undergoing the experimental DBS treatment, one decided to drop out of the trial, one experienced a minor relapse, and two patients, including Buckhalter, have been sober since.
Despite its successes, Dr. Rezai’s DBS surgery is costly, weighing in at around $50,000. Additionally, it must be noted that DBS is not a full cure to drug addiction; patients must use it as supplement to their rehabilitation, with having an encouraging environment as the priority.
“When it comes to staying sober, It’s just as important as the surgery,” said Buckhalter to CNN. He stated that in addition to Dr. Rezai’s treatment, he continues to take an opioid-dependency medication known as suboxone, and attends addiction counselling sessions.
However, National Institute on Drug Abuse Director Nora Volkow believes that regardless of the cost, DBS is still useful towards medical progress.
“Whether or not this goes into the clinic in a meaningful way, it can translate into methods that are less costly and less invasive,” she said in an interview with CNN.
In fact, the current applications of DBS shows how far it has come from its roots. Within the last 30 years, DBS has been practiced in over 200,000 patients with neurological disorders, and has seen very tangible success in some diseases, with over 75 per cent of Parkinson’s patients reporting an increase in symptom manageability due to the treatment.
Recently, DBS implants have also seen a significant improvement in individualized treatment. Whereas older implants require technicians to manually alter treatment protocols, current versions of the implant, like Dr. Rezai’s, allows for a constant support system and treatment altercations without manual intervention.
In the past decade, drug addiction and overdoses have been on an uprise, with roughly a 23 per cent increase in worldwide illicit drug users, from an estimated 240 million in 2011 to an estimated 296 million in 2021. Even after considering the global population growth during this time, the ratio of illicit drug users to global population still increased by a considerable 9 per cent from 2011 to 2021. With DBS implants as a new treatment method for substance abuse disorder, Dr. Rezai hopes to reduce this figure, and plans on advancing the clinical trials to a larger trial group of twelve patients.